Endoscopic Disc Surgery
Endoscopic Disc Surgery
Some causes of back pain such as intervertebral disc protrusion or spinal canal stenosis by putting pressure on the nerves along the spinal canal can lead to pain in the back or legs, numbness or tingling, and weakness in the legs.
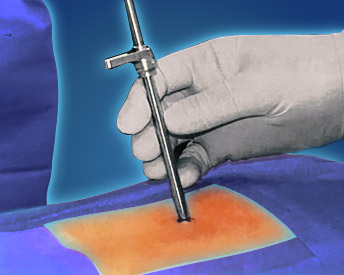
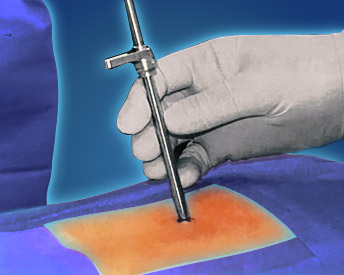
Endoscopic surgery has created a new approach to the treatment of spinal stenosis and disc herniation. This method allows a closer view to the surgical site, and as a result, the accuracy of the surgery is higher. The endoscopic surgery technique causes the least damage to the tissues around the spine and the muscles are less damaged.
Due to minimal tissue damage in this surgical method, endoscopic surgery is associated with less pain (compared to open surgery). Therefore, there is no need for general anesthesia.
Surgery is performed with local or spinal anesthesia (no need for general anesthesia) and an endoscopic camera under a very small skin incision (about 7 mm). Using a narrow tube-like canal, the surgeon enters the desired space, removes the bulging disc or thickened ligament. The duration of the surgery is usually 30 to 45 minutes and the surgical incision is covered with a small dressing.
The patient walks after the anesthesia is removed and is discharged the same day. He is active at home for 5 days and then walks outside.
During the first one to two weeks, a special belt is worn so that the lumbar spine is in a good position during daily activities. After one to two weeks of surgery, the patient can resume his usual work. Lumbar disc endoscopy is performed by transforaminal and interlaminar methods.
For the operation of the fifth and first lumbar intervertebral disc ( L5-S1) in an interlaminar form and at higher levels ( L4-L5) is performed transforaminal.